Abstract
Cognitive impairment (CI) is a serious complication of sickle cell disease (SCD) and can cause significant functional and social limitations. To date, there are only a few studies characterizing CI in adults with SCD. In this study, we comprehensively assessed cognitive function in a cross-sectional sample of patients with SCD compared to healthy controls across ten memory and processing speed domains.
Patients with SCD (HbSS, HbSC and HbS/beta thalassemia) ages 18 years and older were recruited from the University of Pittsburgh Medical Center Adult Sickle Cell Program, and sex- and age-matched controls were recruited from the community and by SCD patient referral. Unlike previous studies, we did not restrict participation to patients with HbSS only and we included all SCD comorbidities. All participants underwent neurocognitive assessments using measures that are validated and accurate in discriminating CI from dementia and normal cognition. We conducted linear regression analyses to estimate the difference in each cognitive domain score between patients and controls. We also contrasted pairwise comparisons between controls and patients with and without stroke, with and without chronic blood transfusions, and classified by disease severity based on genotype.
Among 86 SCD patients and 66 controls, 43% were male and the average age was 36.2 years. SCD patients had fewer years of education on average (13.3 vs. 14.2) and a higher percent had a history of smoking (46% vs. 29%). Additionally, 45% of patients had milder disease (HbSC or HbSb +-thalassemia) with the rest having severe disease (HbSS or HbSb 0-thalassemia)), 14% had a history of stroke, and 20% were receiving chronic exchange transfusions.
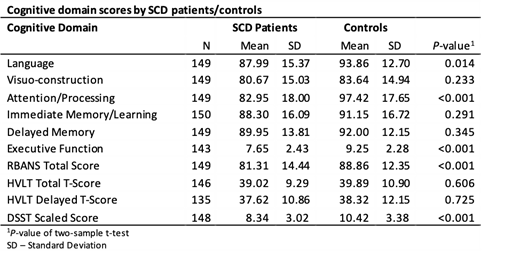
Patients with SCD had significantly lower scores on five out of ten cognitive domains: language (b=-5.88, P=0.014), attention/processing (b=-14.47, P<0.001), RBANS total score (b=-7.55, P<0.001), executive function (b=-1.60, P<0.001), and DSST scaled score (b=-2.08, P<0.001). Adjusting for pre-morbid verbal IQ (VIQ), hemoglobin level, and smoking history, attention/processing (b=-10.70, P=0.001), RBANS total (b=-7.27, P=0.003), and DSST scaled scores (b=-1.54, P=0.019) were significantly lower among patients compared to controls.
In adjusted models, there were no significant differences in cognitive domain scores between patients with mild disease compared to patients with severe disease; both mild and severe disease subgroups had lower attention/processing scores compared to controls (both P<0.05). Patients with SCD and a history of stroke had significantly lower attention/processing, executive function, RBANS total, and DSST scaled scores (all P<0.01) compared to controls, and SCD patients who did not have a history of stroke had lower attention/processing and RBANS total scores than controls (both P<0.05). Patients with a history of stroke had significantly lower executive function (b=-1.65, P=0.012), RBANS total (b=-8.64, P=0.020), and DSST scaled scores (b=-2.43, P=0.015) than patients without a history of stroke. There were no significant differences in cognitive domain scores between patients receiving chronic transfusions and those not receiving transfusions.
To our knowledge, this is the most inclusive real-life study of adult patients with SCD to investigate cognition to date, further characterizing CI among this patient population. Many of the disparities in cognitive function between patients and controls are not explained by pre-morbid VIQ, hemoglobin levels or smoking, indicating further research is needed to understand the pathogenesis of CI in SCD.
Novelli: Novartis Pharmaceuticals: Consultancy.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal